Current applications of precision medicine in intensive care medicine
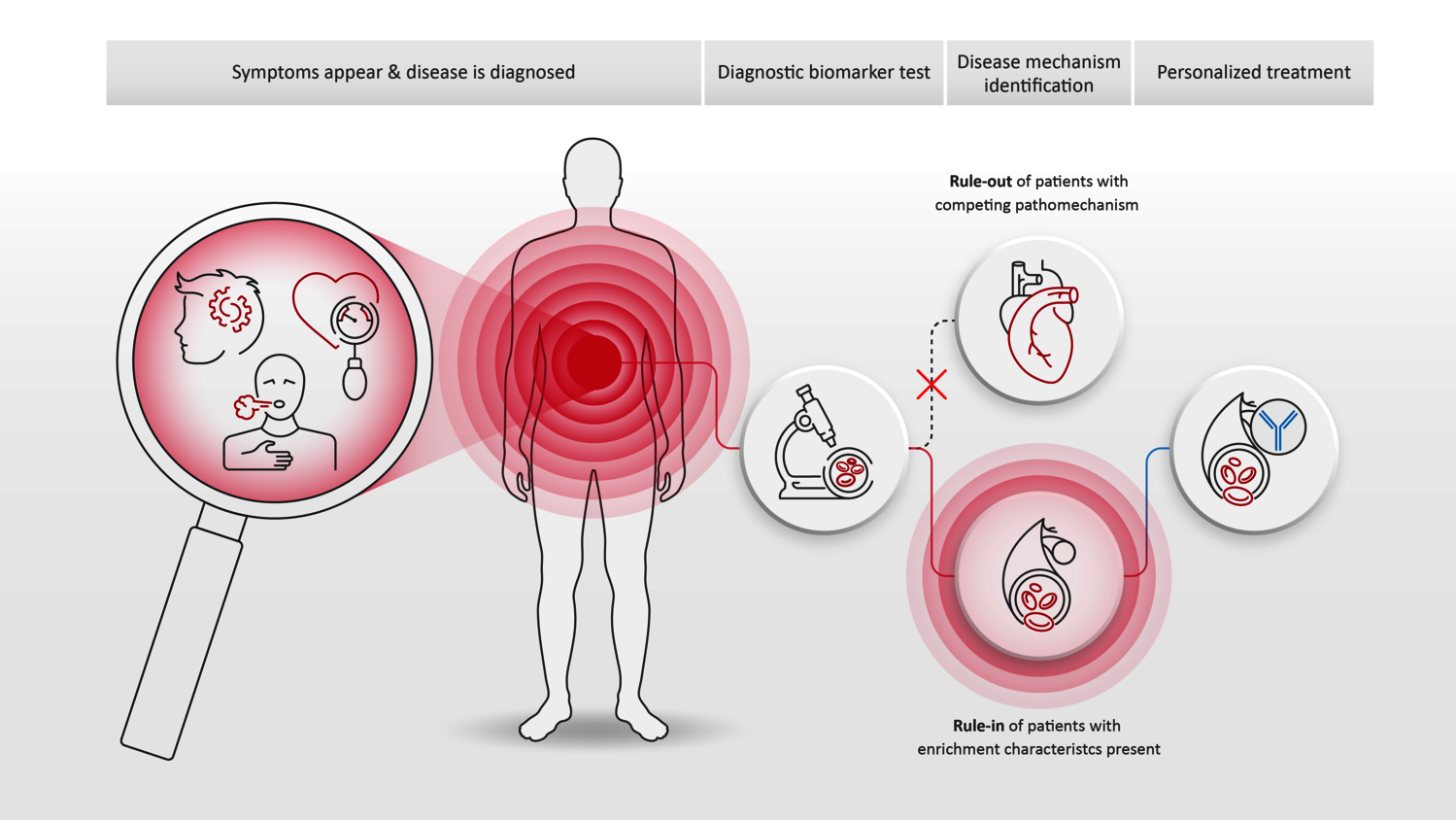
Patients suffering from one particular disease are often treated with the same drug – independent of their age, gender, origin, or even the underlying disease mechanisms, which can vary greatly among different patients. In the field of personalized medicine, these differences are considered with the aim of providing individualized treatment to help the patient with the best possible outcome.
Personalized medicine has already achieved major breakthroughs in the fields of cancer research and cardiology. In the field of intensive care medicine, it remains difficult to identify suitable biomarkers for personalized treatment that can be measured quickly. At the same time, the application is also important, since one and the same disease can often have different underlying causes that require different therapies.
Sepsis and septic shock
Sepsis represents a life-threatening condition resulting from a dysregulated endogenous defense reaction in response to an infection (1). This can result in shock, a life-threatening reduction in blood pressure, and consequently in organ damage and failure.
Septic shock is the most severe form of sepsis, mainly caused by two different disease mechanisms: loss of endothelial function or cardiac depression. The endothelium is the inner membrane of the blood vessel, functioning as a barrier between the blood and the surrounding tissue. Thus, it is regulating blood pressure and the exchange of substances, including oxygen and it preserves blood fluidity. Loss of the endothelial function results in leakage, reduced organs oxygen supply and a dramatic loss in blood pressure. A drastic reduction in blood pressure by cardiac depression, on the other hand, results directly from a reduced pumping capacity of the heart.
By using biomarkers, it is possible to classify the etiology of septic shock. This is important since this allows the development of novel drug candidates in the field of sepsis. Those drug candidates would need to specialize in one disease mechanism respectively, instead of using one drug for all sepsis patients. To detect endothelial dysfunction and exclude cardiac depression, the use of two biomarkers has shown promising results: the hormone bioactive adrenomedullin (bio-ADM) identifies the loss of endothelial barrier function, and the cellular enzyme dipeptidyl peptidase 3 (DPP3) hemodynamic instability resulting in cardiac depression. In a phase-II clinical trial in septic shock, the concept of biomarker-guidance had already been included. The biomarker bio-ADM has been used to enrich the trial patient population and the biomarker DPP3 was applied for data analysis. Results are now integrated in a planned phase III clinical trial in septic shock (2).
Cardiac depression
In cardiac depression (or sudden loss of heart function), the heart is no longer able to supply the body with sufficient blood. If left untreated, it leads to organ failure due to an insufficient supply of oxygen. However, the causes of this disease are also very diverse, instead of a uniform clinical picture. Recent studies show, that uncontrollable cell death e.g., from septic shock, burns, major surgery, or cardiogenic shock, causes the release of DPP3 in the circulation. This disease mechanism is accountable for interruptions of the hormone system which supports heart function.
DPP3 is a bioactive compound, meaning it can be used as biomarker to identify one cause of cardiac depression in shock. If its level in the blood increases, a deterioration of the patient's condition is to be expected. On the other hand, decreasing levels indicate an improvement in the patient's condition. On the other hand, DPP3 could be modulated directly to prevent interruptions of the heart-supporting hormone system. This is where the drug candidate Procizumab applies. It is the first drug candidate in its class to target DPP3 activity that may lead to patient stabilization by inhibiting DPP3 (3).
COVID-19
In patients with severe COVID-19 courses, endothelial barrier dysfunction can be a common secondary complication. Many COVID-19 patients actually develop and die from sepsis (4, 5, 6). Here, also deteriorating of the endothelial barrier leads to vascular leakage, organ dysfunction, and increased mortality. An investigator initiated phase-II clinical trial is now to use biomarkers bio-ADM and DPP3 to identify and enrich COVID-19 patients suffering from endothelial barrier dysfunction. These patients will be treated with the sepsis drug-candidate Adrecizumab to restore and maintain vascular integrity.
References
(1) Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
(2) Geven et al (2019), A double-blind, placebo-controlled, randomised, multicentre, proof-of-concept and dose-finding phase II clinical trial to investigate the safety, tolerability and efficacy of adrecizumab in patients with septic shock and elevated adrenomedullin concentration (AdrenOSS-2), BMJ, doi: 10.1136/bmjopen-2018-024475
(3) Deniau et al (2020) Circulating dipeptidyl peptidase 3 is a myocardial depressant factor: dipeptidyl peptidase 3 inhibition rapidly and sustainably improves haemodynamics, Eur J Heart Fail, doi: 10.1002/ejhf.1601.
(4) Zhou et al (2020), Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet; 395: 1054–62. doi:10.1016/S0140-6736(20)30566-3
(5) Arentz M, Yim E, Klaff L, et al. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA. 2020;323(16):1612–1614. doi:10.1001/jama.2020.4326
(6) Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, Greninger AL, Pipavath S, Wurfel MM, Evans L, Kritek PA, West TE, Luks A, Gerbino A, Dale CR, Goldman JD, O'Mahony S, Mikacenic C. Covid-19 in Critically Ill Patients in the Seattle Region - Case Series. N Engl J Med. 2020 May 21;382(21):2012-2022. doi: 10.1056/NEJMoa2004500.
Disclaimer
The information presented on this blog is meant for health care professionals only. The information provided does not claim to be exhaustive, and is not intended to serve as medical advice, substitute for a doctor’s appointment or be used for diagnosing or treating a disease. For more information please see our Legal Information.