The biomarker penKid is addressing the blind spots in acute kidney injury diagnostics
The current biomarkers used in the critical care routine to detect acute kidney injury (AKI) include serum creatinine and urine output. The limitations of these biomarkers point to insights that are delayed, error prone and unspecific. An emerging body of evidence demonstrates that the biomarker Proenkephalin A 119-159 (penKid*) overcomes these limitations.
Current blind spots of routinely used biomarkers:
- AKI is mostly symptom-free in the early disease stages.
- Current biomarkers show delayed recognition when 50% of kidney function is already lost.
- Standard biomarkers require observation at least at two independent time points.
- Comorbidities, personal factors (e.g. age and muscle mass) and treatments influence currently used biomarkers.
Potential advantages of the kidney function biomarker penKid:
- Showing kidney function in real-time (1).
- Predicting the incidence of AKI within 48h in septic patients (2,3).
- Correlating with the in vivo measurement of glomerular filtration rate (GFR) (4,5,6).
- Reflecting kidney function in adults (7,8,9) and children, representing a biomarker for pediatric AKI (10).
- Independent of inflammation (1,2,3,11) and common comorbidities, e.g. hypertension and diabetes (2).
The biomarker penKid is convincing in clinical research:
A small molecule becomes a messenger for a serious disease
Scientific evidence
The best indicator of kidney function is considered to be the glomerular filtration rate (GFR) (5,7). However, the gold standard technique for determining the true GFR is based on complex, time-consuming, expensive, and invasive interventions using inulin, iothalamate or iohexol that are not feasible in daily practice (13). Today’s routine clinical practice relies on determining an estimated GFR using mathematical formulas (14). However, non-renal factors (age, gender, muscle mass, inflammation, and others) influence the calculation of estimated GFR.
An emerging body of evidence demonstrates that monitoring penKid levels, which indirectly reflect the true glomerular filtration rate (true GFR), overcomes these limitations (4,5,6). PenKid levels reveal kidney function in real-time and offer a blood-based alternative for the complex and time-consuming in vivo measurement of true GFR.
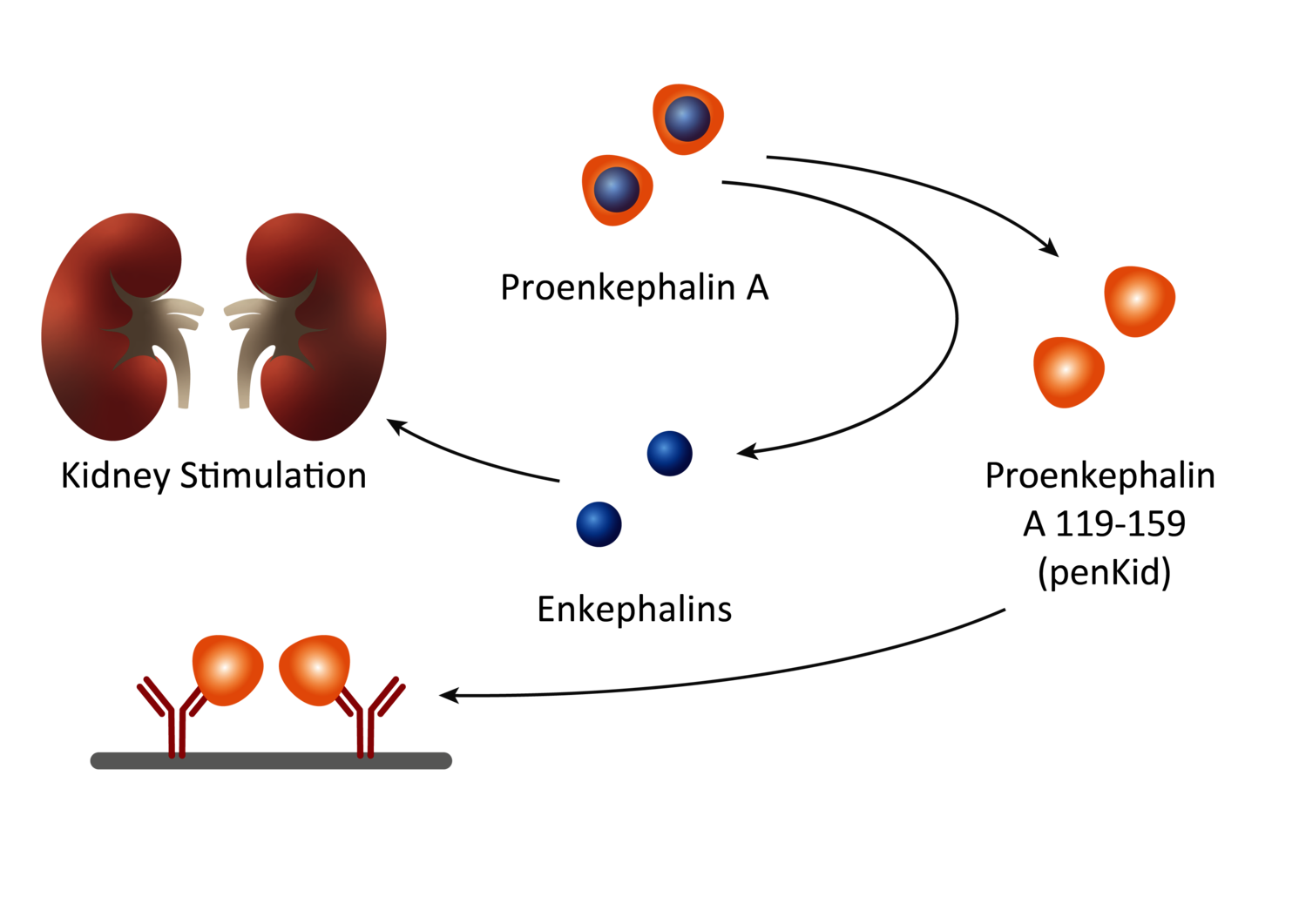
Healthy state
Kidney function is stimulated by the hormone Enkephalin (15) which remains hard to detect. Detecting penKid levels, the stable fragment - Proenkephalin A 119-159 - that results out of the Enkephalin processing, overcomes this limitation.
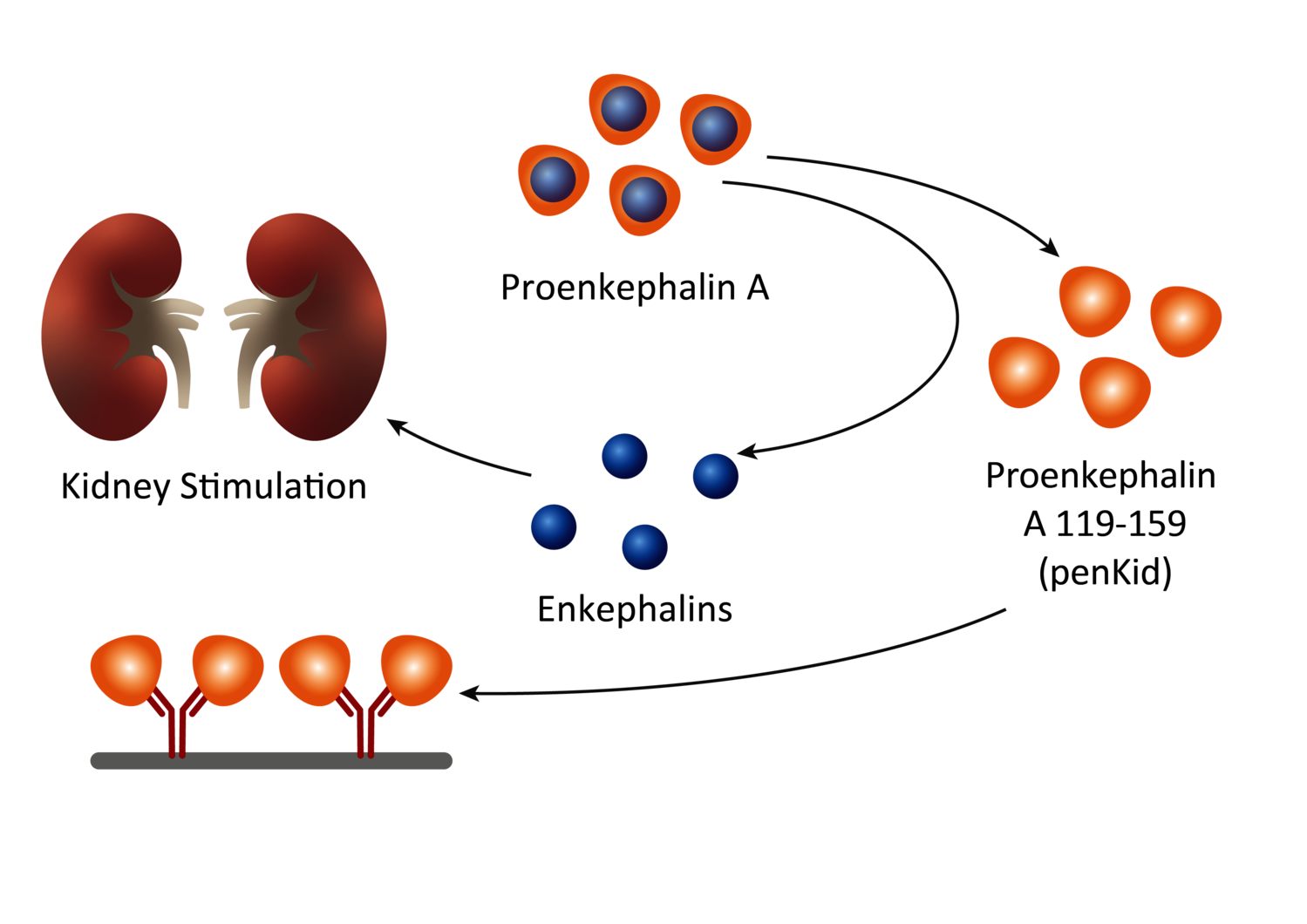
Disease state
The administration of nephrotoxic drugs or critical illness can lead to an impairment of kidney function, which may increase enkephalin production to stimulate renal function, by increasing urine flow and sodium excretion (15). The kidney status can thus be indirectly assessed by measuring penKid blood levels, which reflects kidney function in real-time and remains independent of inflammation (1,2,3,11) and common comorbidities (2).
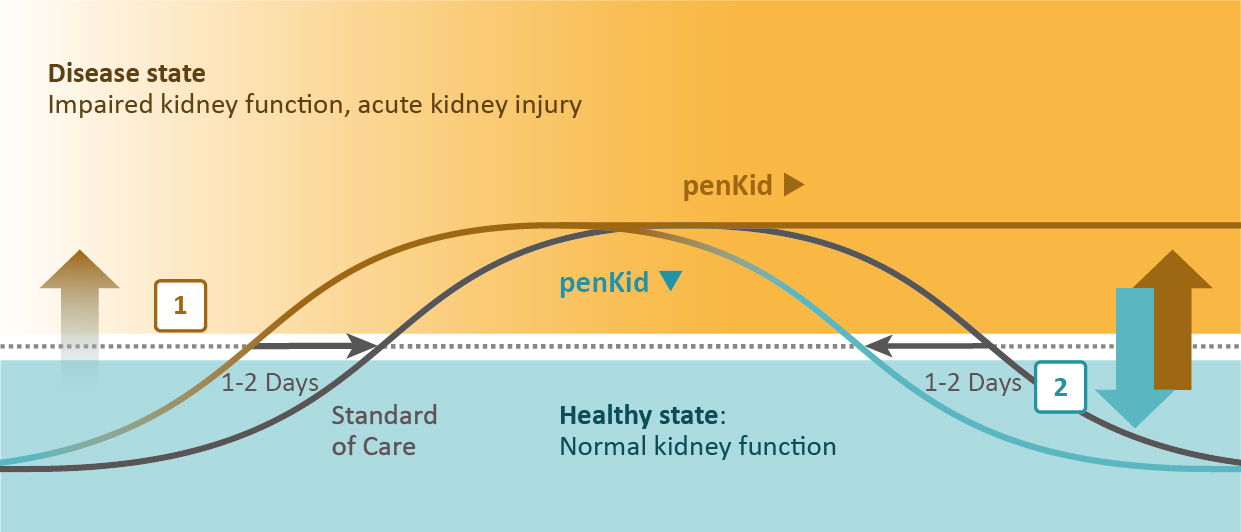
Monitoring kidney function in real-time using the biomarker penKid
Scientific evidence
Independent of common comorbidities (e.g. hypertension and diabetes) and the frequently occurring inflammation in critically ill patients, rising penKid blood levels [1] predict acute kidney injury up to 48 hours earlier than today’s standard of care (16) and decreasing penKid blood levels [2] indicate the improvement of kidney function (2).
Investigated indications
Research disease areas
Sepsis and septic shock
Show more InfoEmergency department (ED): Earlier detection of AKI upon ED admission is an unmet need to stratify patients with AKI timely. PenKid showed great value as an early rule-in or rule-out criteria by effectively detecting the presence and severity of AKI in septic patients with normal serum creatinine levels at admission (1,17).
Intensive care units (ICU): Critically ill patients with sepsis or septic shock admitted to the ICU require efficient management strategies to predict acute kidney deterioration and recovery of renal function. PenKid predicted major adverse kidney events, transient AKI, worsening of renal function, and renal recovery in ICU patients (2,3).
Clinical performance characteristics: 529 adult patients with sepsis or septic shock and available AKI diagnoses were enrolled in a clinical performance study. Performances were computed as the proportion of patients with a clinical diagnosis of AKI within 48 hours after enrolment in the study.
| Parameter | Observed performance |
|---|---|
| Diagnostic sensitivity | 71.8% (95% CI 65.7–77.2%) |
| Diagnostic specificity | 83.1% (95% CI 78.4–86.9%) |
| Positive predictive value (PPV) | 77.1% (95% CI 71.0–82.2%) |
| Negative predictive value (NPV) | 78.8% (95% CI 73.9–83.0%) |
| Diagnostic odds ratio | 12.5 (95% CI 8.2–18.9) |
| Cut-off | 89 pmol/L |
Heart failure
Show more InfoAcute heart failure (AHF): Patients with AHF, renal dysfunction, and inadequate decongestion during hospitalization are at risk of prolonged hospitalization, rehospitalization, and death. The rapid increase of penKid aids in identifying patients who do not tolerate the intensified diuretic therapy and predicts the worsening of renal function, in-hospital mortality, and mortality during follow-up (9,18,19,20).
Chronic heart failure (CHF): There is an unmet clinical need for biomarkers for monitoring patients with CHF, mainly in heart failure with preserved ejection fraction (HFpEF) (i.e., the left ventricle is not filling correctly with blood). High levels of penKid in HFpEF were associated with heart failure rehospitalization (21) and recurrence of acute myocardial infarction (22).
Ambulatory patients: Patients with heart failure have a poor prognosis, but outcomes might be improved by early identification of organ failure risk. Increased penKid levels have shown significant predictive value for risk stratification of stable ambulatory patients (23).
Major surgeries
Show more InfoAKI occurs in up to 40% of patients undergoing cardiac surgery and is a common postoperative complication in complex aortic surgery. Due to its dynamic nature, penKid is a biomarker for the prediction of AKI before and after invasive interventions such as cardiac and aortic surgery (24,25,26).
Organ transplantation
Show more InfoPenKid is associated with kidney function in renal transplant recipients (RTR) and in healthy kidney donors and may be a marker for determining long-term renal prognosis in RTR. High penKid levels are associated with an increased risk of graft failure and may indicate an additional benefit of penKid in the early identification of RTR at risk of graft failure (27).
Renal replacement therapy
Show more InfoCritically ill patients are often at risk of developing AKI and are likely in need of organ support, such as renal replacement therapy (RRT) (30). However, the most effective timing to start RRT remains uncertain. PenKid levels have been shown to predict the need for RRT on day one or later during hospitalization in sepsis patients (3,28) as well as in liver transplant patients (16). The ELAIN and RICH studies scientifically proved that penKid remains informational during RRT, indicating kidney function recovery and supporting the decision to stop RRT/CRRT (31, 32) safely.
Burned patients
Show more InfoPenKid levels in patients on admission to the ICU were associated with the risk of developing AKI in patients with severe burns, where mortality rates range from 30-70%. The data suggest that penKid levels could provide additional value to the currently available markers of renal function and AKI to better quantify kidney function in critically ill patients (12).
Pediatric ICU
Show more InfoPediatric AKI is often diagnosed too late for successful therapeutic interventions, leading to adverse outcomes and chronic kidney impairment (31). PenKid identifies AKI in infants and offers a potential solution to the shortcomings in pediatric critical care. Considering higher reference values in critically ill children under two years of age, high or increasing penKid concentrations predict AKI and its severity (10).
Chronic kidney disease / Contrast-induced nephrotoxicity
Show more InfoIodinated contrast media administration is one of the most important triggers of AKI in hospitalized patients (30). PenKid levels improve the early detection of contrast‐induced AKI in chronic kidney disease patients and accelerate AKI detection by 24 hours (8).
*Disclaimer
Sphingotest® penKid®, sphingotest® bio-ADM® are offered for research use only. “penKid” and “bio-ADM” represent the analytes Proenkephalin A 119-159, and bioactive Adrenomedullin 1-52 respectively.
Reference Literature
(1) Marino et al. (2015), Diagnostic and short-term prognostic utility of plasma proenkephalin (pro-ENK) for acute kidney injury in patients admitted with sepsis in the emergency department, J Nephrol,
View the paper
(2) Hollinger et al. (2018), Proenkephalin A 119-159 (Penkid) is an early biomarker of septic acute kidney injury - the kidney in sepsis and septic shock (Kid-SSS) study, Kidney Int Rep.
View the paper
(3) Caironi et al. (2018), Circulating Proenkephalin, Acute Kidney Injury, and Its Improvement in Patients with Severe Sepsis or Shock. Clin Chem.
View the paper
(4) Beunders et al. (2017), Proenkephalin (PENK) as a novel biomarker for kidney function, JALM.
View the paper
(5) Beunders et al. (2020), Proenkephalin compared to conventional methods to assess kidney function in critically ill sepsis patients, Shock.
View the paper
(6) Khorashadi et al. (2020), Proenkephalin: A New Biomarker for Glomerular Filtration Rate and Acute Kidney Injury. Nephron.
View the paper
(7) Donato et al. (2018), Analytical performance of an immunoassay to measure proenkephalin. Clin Biochem.
View the paper
(8) Schulz et al. (2017), High Level of Fasting Plasma Proenkephalin-A Predicts Deterioration of Kidney Function and Incidence of CKD. J Am Soc Nephrol.
View the paper
(9) Emmens et al. (2019), Proenkephalin, an Opioid System Surrogate, as a Novel Comprehensive Renal Marker in Heart Failure. Circ Heart Fail.
View the paper
(10) Hartman et al. (2020), Proenkephalin as a new biomarker for pediatric acute kidney injury - reference values and performance in children under one year of age. Clin Chem Lab Med.
View the paper
(11) Kim et al. (2017), Proenkephalin, Neutrophil Gelatinase-Associated Lipocalin, and Estimated Glomerular Filtration Rates in Patients With Sepsis. Ann Lab Med.
View the paper
(12) Dépret et al. (2020), PenKid measurement at admission is associated with outcome in severely ill burn patients. Burns.
View the paper
(13) Bjornstad et al. (2018), Measured GFR in Routine Clinical Practice-The Promise of Dried Blood Spots. Adv Chronic Kidney Dis.
View the paper
(14) Schaeffner (2017), Determining the Glomerular Filtration Rate-An Overview. J Ren Nutr.
View the paper
(15) Sezen et al. (1998), Renal Excretory Responses Produced by theDelta Opioid Agonist, BW373U86, in Conscious Rats. Journal of Pharmacology and Experimental Therapeutics.
View the paper
(16) Lima et al. (2022), Role of proenkephalin in the diagnosis of severe and subclinical acute kidney injury during the perioperative period of liver transplantation. Pract Lab Med.
View the paper
(17) Rosenqvist et al. (2019), Proenkephalin a 119-159 (penKid) - a novel biomarker for acute kidney injury in sepsis: an observational study. BMC Emerg Med.
View the paper
(18) Molvin et al. (2019), Bioactive adrenomedullin, proenkephalin A and clinical outcomes in an acute heart failure setting. Open Heart.
View the paper
(19) Ng et al. (2017), Proenkephalin, Renal Dysfunction, and Prognosis in Patients With Acute Heart Failure: A GREAT Network Study. J Am Coll Cardiol.
View the paper
(20) Matsue et al. (2017), Clinical Correlates and Prognostic Value of Proenkephalin in Acute and Chronic Heart Failure. J Card Fail.
View the paper
(21) Kanagala et al. (2019), Proenkephalin and prognosis in heart failure with preserved ejection fraction: a GREAT network study. Clin Res Cardiol.
View the paper
(22) Ng et al. (2014), Proenkephalin and prognosis after acute myocardial infarction. J Am Coll Cardiol.
View the paper
(23) Arbit et al. (2016), Prognostic Usefulness of Proenkephalin in Stable Ambulatory Patients With Heart Failure. Am J Cardiol.
View the paper
(24) Shah et al. (2015), Proenkephalin predicts acute kidney injury in cardiac surgery patients. Clin Nephrol.
View the paper
(25) Mossanen et al. (2017), Elevated Soluble Urokinase Plasminogen Activator Receptor and Proenkephalin Serum Levels Predict the Development of Acute Kidney Injury after Cardiac Surgery. International Journal of Molecular Sciences.
View the paper
(26) Gombert et al. (2020), Proenkephalin A 119-159 May Predict Post-operative Acute Kidney Injury and in Hospital Mortality Following Open or Endovascular Thoraco-abdominal Aortic Repair. Eur J Vasc Endovasc Surg.
View the paper
(27)Benning L et al. (2025) Proenkephalin A 119-159 in Kidney Transplantation: A Novel Biomarker for Superior Tracking of Graft Function Trajectories. Transpl. Int.
(28) Kim et al. (2020), Proenkephalin Predicts Organ Failure, Renal Replacement Therapy, and Mortality in Patients with Sepsis. Ann Lab Med.
View the paper
(29) Andreoli (2009), Acute kidney injury in children. Pediatr Nephrol.
View the paper
(30) Ali et al. (2018), The Prevention and Management of Contrast-induced Acute Kidney Injury: A Mini-review of the Literature. Cureus.
View the paper
(31) von Groote et al. (2022), Proenkephalin A 119-159 predicts early and successful liberation from renal replacement therapy in critically ill patients with acute kidney injury: a post hoc analysis of the ELAIN trial. Crit Care.
View the paper
(32) von Groote et al. (2023), Evaluation of Proenkephalin A 119-159 for liberation from renal replacement therapy: an external, multicenter pilot study in critically ill patients with acute kidney injury. Crit Care.
View the paper